Psychoneuroimmunology:
The Science Connecting Body and Mind
Published by SHAMIR -
www.borhatorah.org
Yakir Kaufman, MD
The Torah gave the world an understanding of the reciprocal
connections between body and soul. Until recently, many scientists rejected
the concept that psychological factors and well-being can affect health and
disease. In part, this may been caused by a lack of technological tools to
prove these links. During the last decade, new methods and findings in
neuroscience, neuroimaging, and molecular biology have discovered
connections between emotions and disease, between the brain and the immune
system, the mind and the body. Science and medicine are beginning to become
aware of this interplay. The
psycho-neuro-immunology
(PNI) revolution uplifts science from a mechanistic, dualistic,
reductionistic Descartian view of the human state to a more integrative
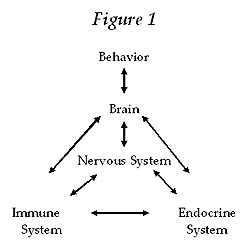
perception of the complexity and beauty of human existence. PNI deals with
the interactions among the mind, human behavior, the nervous system, the
immune system, and the endocrine system. Understanding these complex
interactions is essential for gaining a better understanding on how to
maintain health and to prevent and treat disease. PNI guides science to the
holistic view of body and soul interaction found in the Torah.
Yakir
Kaufman was born in Haifa and received his MD from the Hebrew
University Hadassah Faculty
of Medicine in 1994. In 1995 he become a resident doctor at the department
of neurology of the Hadassah University Hospital in Jerusalem. Dr. Kaufman
is a member of the Israeli Neurological Society and a junior member of the
American Academy of Neurology. With his wife and children, he is currently
in Toronto,
Canada, where he has been appointed a Fellow in the Behavioural Neurology
Program at the Baycrest Centre for Geriatric Care and the Rotman Institute.
His areas of research include psychoneuroimmunology and the link between
spirituality and health.
Mind-Body Unity: Science Is Catching Up with the Torah
The Torah
gave the world an understanding of the reciprocal connections between body
and soul. Genesis describes the creation of Adam as the implant of a
heavenly soul into an earthly body. Throughout the Torah the human
interaction between heavenly soul and animal body is an overriding theme.
This interaction is a cornerstone of the Torah perception of life.
Moses
Maimonides, the great Torah authority and physician, states in the third
chapter of his Regime of Health that his
medical system is based on the Torah concept of a �healthy soul in a healthy
body.�1 Maimonides expanded the Latin
aphorism of �a healthy mind in a healthy body.� Whereas Greek and Roman
medicine, as formulated by Galen, tried to treat the psyche as an isolated
system in cases of mental illness, Maimonides emphasized the necessity of
treating the spiritual aspect of every condition of every patient. He
understood that the physical well-being of a person is dependent on mental
well-being, and reciprocally, that mental well-being is dependent on
physical well-being. Furthermore, in the
Mishneh Torah,
Hilkhot Deot
4:1 Maimonides states that health is necessary in order to know G-d,
which is the highest purpose in life.
Throughout
the generations, similar concepts have been expressed by numerous Torah
commentators. In the past century, the Baal
Shem Tov and his hasidic followers emphasized
and revitalized this approach. The Maggid of Mazritch says, �A small hole in
the body is a big hole in the soul.�
In our
generation, the Lubavitcher Rebbe, Rabbi Menachem Mendel Schneerson, wrote
to a conference of Torah observant physicians in New York in 1992, �physical
health depends upon the health of the nefesh
(soul)�the more healthy the nefesh is, the more it can guide the body to
mend its deficiencies� (Igrot Kodesh, volume
11, page 202).
Science and
medicine are beginning to awaken from a long unawareness concerning the
interplay between bodily factors and the mind and soul. In this sense, we
are lucky to be living in an exciting era, when the discipline of psycho-neuro-immunology
(PNI) is pioneering a revolution in elevating medicine from a mechanistic,
dualistic Descartian perception of the human condition to a new paradigm
embracing the complexity and beauty of human existence.
The old
reductionistic perception of the human being as the sum of many separate
biological systems is rooted in ancient Greek philosophy. The difficulty of
Western medicine in effectively treating many disease states, especially
chronic diseases, may be related to this narrow, non-integrative concept.
This attitude also incurs dissatisfaction from health service clients.
Patients feel they are looked upon by ultra-specialists as a compilation of
systems and not as an integrated human being.
In contrast
to the view that body systems function separately, technological development
in neuroimaging and molecular biology show that systems continuously
interact among themselves. Understanding these complex interactions is
essential for gaining a better perception on how to maintain health and
prevent and treat disease.2 This perception
may lead to the remodeling health-care.
New
and Ancient
Today�s
exponential growth in technology has allowed us to perceive and understand
the human body and brain as we have never done before. We can now �see� the
brain while it is engaged in the most delicate tasks. Technological
breakthroughs in neuroimaging, such as positron emission tomography (PET),
functional magnetic resonance (FMRI), and single photon emission
computerized tomography (SPECT), give us a first-time opportunity to
pinpoint areas of the brain that are responsible for the generation of
emotions, thoughts, and even higher abilities of the mind, such as
meditation and prayer.3, 4
Another
area of technological advancement that has boosted the understanding of the
connection between body and mind is molecular biology. Molecular biology has
given us the opportunity to track down minute quantities of substances
traveling through the human body and interacting with different systems of
the body. Of great significance are the molecules found interacting in the
brain, especially the limbic system responsible for our emotions, with other
bodily systems. The increasing ability to track the pathways of minute
amounts of molecules and monitor their effect on different systems has
enhanced our knowledge of how mental, emotional, or spiritual changes can
alter the molecular profile of the immune or hormonal system and thus affect
the body.5,6
Today, PNI
through molecular biology techniques provides evidence that
behavioral/psychological factors�primarily stress�can impair immunological
reactivity.7, 8, 9, 10, 11 Conversely,
studies in PNI have demonstrated that reduction of stress can enhance immune
function in its task of protecting the body from infections, cancer, and
other disease states.12, 13,
14, 15, 16, 17, 18
Hence, as
more interactions between bodily systems are being discovered, science
better understands how changes in a person�s mental, emotional, or spiritual
state can change the molecular profile of his or her immune or hormonal
system, and thus affect the body.
Thus,
science today is approaching the Torah understanding that state of mind
affects physical health and disease.
Torah, PNI, and the Definition of Health
You will then serve G-d your L-rd, and he will bless your bread and your
water. I will remove sickness from among you�. I will make you live out full
lives. (Exodus 23: 25-26)
The ancient
but vital Torah concept of health expressed by Maimonides as a �healthy soul
in a healthy body� has been recognized by science only in the last century.
According to the modern definition of health, as defined by the World Health
Organization:
Health is a complete state of physical, social, and mental well-being and
the mere absence of disease or infirmity.19
�Mental
well-being� means both psychological and spiritual well-being. Health by
this definition is considered primarily an outcome of a person�s state of
well-being. Spiritual well-being is an important component of general
well-being.20 Whereas a deterioration of
well-being may bring disease, enhancement of well-being may prevent disease
or augment cure. Thus, the concept of the mind-body relationship as defined
in the Torah and rediscovered by PNI is embedded in the current definition
of health.
Stress and Disease
Psychoneuroimmunology deals
with the interactions among the mind, behavior, the nervous system, the
immune system, and the endocrine system.
One of the foci of PNI is the study of the stress phenomenon and its harmful
influence on the body, resulting in disease. Chronic stress, and its ill
effects is an example of the connection between body and mind. The cause of
disease is multi-factorial. It has been established that chronic stress is a
risk factor in the leading causes of morbidity and mortality. Chronic stress
has been shown to be a risk factor in heart disease, stroke, cancer,21,
22, 23 infection, 24, 25, 26 wound
healing,27 autoimmune disease,28,
29 depression,30, 31, 32
infertility,33, 34, 35, 36, 37, 38 pain,
and many other disease states.
Stress has
many definitions. A relevant one for our discussion is that stress is an
extraordinary demand on physiological and psychological defenses and
adaptation mechanisms with concomitant neuro-immuno-endocrine responses.
Stress
elicits a �fight or flight� (Hans Selye) reaction. This reaction is
essential in animals and humans for survival, particularly when encountered
by danger. The confronted organism can quickly recruit tremendous energy to
overcome danger either by fighting or fleeing the source of danger.
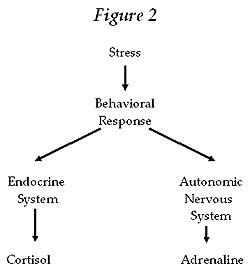
The stress
response mechanism is manifested in two major pathways (see Figure 2).
First, the endocrine pathway causes secretion of several stress hormones,
including CRH, ACTH, and cortisol. Cortisol has a potent, wide range effect
on many organs. After being secreted, it is distributed throughout the body
via the bloodstream. It enters the cells and affects the DNA within the
cellular nucleus, thus changing the functioning of the cells, organs, and
bodily systems.
The
second pathway is the autonomic pathway, involving activation of the
sympathetic nervous system that stimulates the adrenal gland to secrete
adrenaline. Adrenaline, like cortisol, has a large array of effects on
several systems.
The
significant changes following stress, although favorable on the short term,
have a high cost when repeatedly activated on the long run (i.e., chronic
stress). The stress response weakens the immune system�s ability to resist
disease. Thus, stress exposes us to reduced resistance. An ever-increasing
scientific database reveals that chronic stress is a risk factor for many
disease processes. Various studies indicate that stress events or breakdown
of psychological defenses are related to the onset of allergic, autoimmune,
infectious, neoplastic, gastrointestinal, cardiovascular, and other
illnesses. Other studies tie stress with myocardial infarctions (heart
attacks), stroke, cancer, hypertension, diabetes, arthritis, infertility,
depression, obesity, and many more problems. The first three illnesses
listed above are the main cause of morbidity and mortality in Western
societies today. This means that stress, by causing a �negative� mind-body
interaction, is a significant factor in morbidity and mortality.
The cause
of disease is multi-factorial. Why is it that while individuals within a
group of people (e.g., a family) may have a common genetic tendency to
develop a disease, only some of them will actually develop the illness while
others won�t? And why is it that virulent bacteria can be found in certain
people, of whom only a few will actually become infected and sick? These two
examples show us that diseases are caused by factors other than just a
certain genetic background or the mere presence of an infective agent (e.g.,
bacteria or virus). The decline of immune function through stress may be
responsible for the ability of the bacteria to cause infection or of a
genetic trait to become expressed as an actual disease.
Stress and Health: A Two-Way Street
Rebbe Nahman
of Breslov said, �If you believe you can damage, then believe you can mend.�
Studies
have repeatedly demonstrated that stress reduction can boost the immune
system, enhance well-being, and reduce morbidity and mortality risk.
Rebbe Nahman�s
counsel that we can mend as well as damage ourselves is paralleled in the
functioning of the stress mechanism. Amazingly, the same mind-body mechanism
that causes disease can work in the reverse direction and enhance health.
Numerous studies have shown that stress reduction and the enhancement of
well-being can boost the immune system and prevent disease. This means that
the same physiological mechanism connecting body and mind can work both
ways. The same mechanism can either cause disease through chronic stress or
reverse its harmful effects through reducing stress and augmenting
well-being.
We can
better appreciate this two-way process by acknowledging the placebo
phenomenon. A placebo drug is a substance that has no pharmaceutical impact
but nonetheless may actually cause a desired effect quite like that of a
�real� drug. Most drugs have been approved for use through a process proving
that its �sister� placebo drug actually had an effect. During the process of
developing new drugs the placebo effect becomes a �problem� because there
may not be a significant difference between the clinical effect of the
�real� drug and that of the placebo. Some scientists argue that certain
medications (e.g., anti-depressants) are effective mainly because of their
placebo effect.
What
underlies the placebo phenomenon? How can a mere �nothing� pill cure? The
placebo phenomenon seems to reveal the power of suggestion. Is it a trigger
for the mind to actualize an internal potential mechanism to cure the body?
Does it show an intrinsic ability of the mind to heal the body? The placebo
is an example of how it is possible for the mind to initiate a curing
process from within. The placebo phenomenon is an extraordinary illustration
of the therapeutic potential of the mind-body relationship when directed in
a constructive direction. With the right set of mind a person can improve
his or her physical condition. Numerous studies have shown this. Reduction
of stress through a wide range of strategies and techniques can reduce
morbidity and enhance the immune function to provide protection from
disease.
Is
Modern Medicine Targeted to Enhance Health?
The big
question is: If health is an outcome of well-being, then shouldn�t the
primary goal of any health system be the enhancement of well-being? Wouldn�t
a preventive medical policy through enhancement of physical, social, and
mental well-being be cost-effective? Is modern medicine inducing well-being?
And if not, why not? Many modern medicine patients feel that their
well-being decreases after an encounter with medical services.
There seems
to be an unwritten, silent agreement between patients and physicians saying:
When the patient comes to the physician with a complaint of a symptom, the
physician gives the patient a drug or surgery to relieve the symptom.
Although this relative relief of the symptom has its benefit, it does not
address the true underlying process that caused the disease to surface.
Studies have shown that certain medications that improved laboratory test
results in certain patients are liable to reduce well-being and on the whole
diminish health outcomes.39, 40
Modern
medical research has a tremendous mass of data on how to prevent disease and
to enhance health. Much more could be done to enhance well-being and prevent
disease (primary and secondary prevention). We lag behind in educating the
public about risk factors such as stress and its adverse effects. The public
should know that stressful lifestyles may be risk factors for disease.
Contemporary medicine is not primarily focused on preventing disease but on
treating disease after it has appeared. This focus makes the treatment more
costly and incomplete. Western health policy is building the proverbial
hospital under a broken bridge instead of fixing the bridge.
The West
could learn from China. In the past, the Chinese government paid subsidies
to health professionals if the community for which they were medically
responsible was physically well. This economic incentive actively enhanced
preventive medicine. In our society, physicians are usually financially
rewarded if they have more patients (and sometimes rewarded if they treat
their patients with more drugs and surgical procedures). This causes a
reversed incentive. Physicians today have a �heroic� role to save patients
suffering from life-threatening maladies. Preventive care to avoid disease
in the first place is considered much less heroic. It is also less
financially rewarding.
How
to Reduce Stress and Enhance Health
What is the
best, most long-lasting way to reduce stress and thus to enhance health? It
is clear that any symptomatic or superficial solution will be short-acting
and will have side effects (such as those given by anxiolytic drugs and
benzodiazepines).
When new
findings concerning the mind-body connection are acknowledged, then we may
conclude that the most profound way to reduce stress is through changing our
state of mind. To do this calls for deep, thorough, long-term introspective
work. It takes serious and consistent effort to change a state of mind that
has produced stress for many years into a different state of mind, but it is
possible to succeed.
Of course,
appropriate guidance is needed to go through such a complex, profound but
gradual change. If the mind is in constant turmoil and internal conflict,
the body also will not be at peace, and disease might eventually appear. If
anxiety, sadness, anger, dissatisfaction persist, these eventually will take
their toll on the immune, nervous, and endocrine (hormonal) systems and
bring about either mental or physical disease.
A profound
solution for this common situation is a conscious continuous learning
process of how to restore psychological, social, and spiritual well-being.
It is possible to learn how to restore long-lasting and true inner peace and
happiness. It takes dedication and time, but it�s definitely worth the
while. The body will benefit from this mindful effort. Our Talmud sages
said, �As the effort, so is the reward.�
When the
Maggid of Mazritch says, �A small hole in the body is a big hole in the
soul,� he is teaching us that to mend the body, we must first mend the soul.
Health comes about through a continuous quest to improve psychological and
spiritual well-being.
New
Model for Health Care
Healthcare
systems and physicians can easily integrate these new understandings in
their practice. Actually, good medicine based on mind-body interactions is
cost-effective and can save society tremendous unnecessary expenses. Public
money is wasted by building hospitals under broken bridges. A society that
places top priority on enhancing the well-being of its population, rather
than on waging technological wars against advanced stages of disease, can
dramatically cut its medical budget and create a healthier society.
Physicians
and other health professionals should discuss issues of well-being with
their patients. By both assessing well-being and stress factors in the
clients and prescribing therapies and strategies to reduce stress, doctors
can enhance the physical, social, psychological, and spiritual well-being of
their clients. Physical and mental disease can be prevented.
From
Treating Symptoms to Achieving Health: Where Mind and Matter Meet
If we
acknowledge the evidence showing the connection between mind and body, we
can then understand that inner stress, turmoil, or conflict is the source of
many maladies. Therefore, only by addressing these issues can the healing
process be complete. Only then is the solution a profound cure and not
merely symptomatic or superficial temporary measures. This more inclusive
approach demands the active participation of the patient. The therapist can
offer guidance, but it�s the patient who does the work (in contrast to
surgery or medication, where the patient is more passive).
As Jews we
have the merit and obligation to bring the light of G-d and the Torah down
into every aspect of this world. The Torah guides every aspect of our
lives�action, ethics, and morals. If we dwell deeply in the Torah, we can
find guidance for our search for a better health care system and optimize
our medical practice and our own well-being and health. We must take
advantage of the great opportunity brought by the new profound scientific
understanding of the physiology of mind-body interactions to remodel our
practice of medicine. The advancement in scientific understanding, aided by
the enormous progress made in medical technology, brings science closer to
the Torah paradigm of the connection between mind and body. The reciprocal
mind-body connection is the core of physical, social, psychological, and
spiritual well-being in health.
There is a
long called for need for quality medical professionals who have a complex
integrative understanding of mind-body interactions. There is a need for
healthcare workers dedicated to enhancing the well-being of their clients. A
responsible medical system can guide the individual and society to physical,
social, psychological, and spiritual well-being.
Part Two will discuss spiritual well-being and health.
RELATED ARTICLES:
 Genesis & The Big Bang Theory by
Dr. Gerald Schroeder from
AishAudio.com
Genesis & The Big Bang Theory by
Dr. Gerald Schroeder from
AishAudio.com
 Scientific Data Supporting Creation
by
Mr. Harold Gans
from AishAudio.com
Scientific Data Supporting Creation
by
Mr. Harold Gans
from AishAudio.com
 Signature of God
by
Mr. Harold Gans
from AishAudio.com
Signature of God
by
Mr. Harold Gans
from AishAudio.com
 The Fine
Tuning of the Universe
The Fine
Tuning of the Universe
 The Moral
Approach to God's Existence
The Moral
Approach to God's Existence
 The
Theological implications of Modern Cosmology
The
Theological implications of Modern Cosmology
 Nature Reveals
Design
Nature Reveals
Design
 Search For
Truth
Search For
Truth
 Science
Quotes
Science
Quotes
 Neurology and The Soul
Neurology and The Soul
 The Cohanim / DNA Connection
The Cohanim / DNA Connection
 The
Anthropic Principle
The
Anthropic Principle
Notes
1
Maimonides, Regimen of Health (1198) chapter 3.
See Fred Rosner, Medical Encyclopedia of Moses
Maimonides (Northvale, NJ: Jason Aronson, 1998) item �Psychosomatic
Medicine� pp. 183-184.
2
E.M. Sternberg, �Does Stress Make You Sick and Belief Make You Well? The
Science Connecting Body and Mind� in Ann NY Acad Sci
(vol. 917, 2000) pp. 1-3.
3
A.B. Newberg and J. Iversen, �The Neural Basis of the Complex Mental Task of
Meditation: Neurotransmitter and Neurochemical Considerations� in
Med Hypotheses (vol. 61, 2003) pp. 282-291.
4
A. Newberg, A. Alavi, M. Baime, M. Pourdehnad, J. Santanna, E. d�Aquili,
�The Measurement of Regional Cerebral Blood Flow during the Complex
Cognitive Task of Meditation: A Preliminary SPECT Study� in
Psychiatry Res (vol. 106, 2001) pp. 113-122.
5
J.K. Kiecolt-Glaser, L. McGuire, T.F. Robles, and R. Glaser,
�Psychoneuroimmunology and Psychosomatic Medicine: Back to the Future� in
Psychosom Med (vol. 64:1, 2002) pp. 15-28.
6
J.K. Kiecolt-Glaser and R. Glaser, �Psychoneuroimmunology and Health
Consequences: Data and Shared Mechanisms� in Psychosom
Med (vol. 57:3, 1995) pp. 269-274.
7
J.K. Kiecolt-Glaser, L. McGuire, T.F. Robles, and R. Glaser,
�Psychoneuroimmunology and Psychosomatic Medicine: Back to the Future� in
Psychosom Med (vol. 64:1, 2002) pp. 15-28.
8
W.B. Malarkey, J.K. Kiecolt-Glaser, D. Pearl, and R. Glaser, �Hostile
Behavior during Marital Conflict Alters Pituitary and Adrenal Hormones� in
Psychosom Med
(vol. 56:1, 1994) pp. 41-51.
9
J.K.
Kiecolt-Glaser, J.T. Cacioppo, W.B. Malarkey, and R. Glaser, �Acute
Psychological Stressors and Short-Term Immune Changes: What, Why, for Whom,
and to What Extent?� Psychosom Med (vol. 54:6,
1992) pp. 680-685.
10
J.K. Kiecolt-Glaser, R. Glaser, E.C. Shuttleworth, C.S. Dyer, P. Ogrocki,
and C.E. Speicher, �Chronic Stress and Immunity in Family Caregivers of
Alzheimer�s Disease Victims� in Psychosom Med
(vol. 49:5, 1987) pp. 523-535.
11
J.K. Kiecolt-Glaser, L.D. Fisher, P. Ogrocki, J.C. Stout, C.E. Speicher, and
R. Glaser, �Marital Quality, Marital Disruption, and Immune Function� in
Psychosom Med (vol. 49:1, 1987) pp. 13-34.
12
B.A. Esterling, J.K. Kiecolt-Glaser, and R. Glaser, �Psychosocial Modulation
of Cytokine-Induced Natural Killer Cell Activity in Older Adults� in
Psychosom Med (vol. 58:3, 1996) pp. 264-272.
13
J.K. Kiecolt-Glaser, W. Garner, C. Speicher, G.M. Penn, J. Holliday, and R.
Glaser, �Psychosocial Modifiers of Immunocompetence in Medical Students� in
Psychosom Med (vol. 46:1, 1984) pp. 7-14.
14
G.F. Solomon, �Physiological Responses to Environmental Design:
Understanding Psychoneuroimmunology (PNI) and Its Application for
Healthcare� in J. Health Des (vol. 8, 1996) pp.
79-83.
15
G.F. Solomon, �Whither Psychoneuroimmunology? A New Era of Immunology, of
Psychosomatic Medicine, and of Neuroscience� in Brain
Behav Immun (vol. 7:4, 1993) pp. 352-366.
16
G.F. Solomon and A.A. Amkraut, �Psychoneuroendocrinological Effects on the
Immune Response� in Annu Rev Microbiol (vol.
35, 1981) pp. 155-184.
17
G.F. Solomon and R.H. Moos, �Psychologic Aspects of Response to Treatment in
Rheumatoid Arthritis� in GP (vol. 32:6, 1965)
pp. 113-119.
18
R.H. Moos and G.F. Solomon, �Personality Correlates of the Degree of
Functional Incapacity of Patients with Physical Disease� in
J. Chronic Dis (vol. 18:10,
1965) pp. 1019-1038.
19
Preamble to the Constitution of the World Health Organization, as adapted by
the International Health Conference, New York, 19-22 Jun 1946, signed on 22
Jul 1946 by the representatives of sixty-one states (Official
Records of the World Health Organization, no. 2, p. 100) and entered
into force on 7 Apr 1948.
20
E.L. Idler and S.V. Kasl, �Religion among Disabled and Nondisabled Persons
I: Cross-Sectional Patterns in Health Practices, Social Activities, and
Well-Being� in J Gerontol B Psychol Sci Soc Sci
(vol. 52:6, 1997) S294-S305.
21
S. Ben Eliyahu, G.G. Page, R. Yirmiya, and G. Shakhar, �Evidence that Stress
and Surgical Interventions Promote Tumor Development by Suppressing Natural
Killer Cell Activity� in Int J Cancer (vol.
80:6, 1999) pp. 880-888.
22
S. Ben Eliyahu, R. Yirmiya, J.C. Liebeskind, A.N. Taylor, and R.P. Gale,
�Stress Increases Metastatic Spread of a Mammary Tumor in Rats: Evidence for
Mediation by the Immune System� in Brain Behav Immun
(vol. 5:2, 1991) pp. 193-205.
23
S. Ben Eliyahu, R. Yirmiya, Y. Shavit, and J.C. Liebeskind, �Stress-Induced
Suppression of Natural Killer Cell Cytotoxity in the Rat: A Naltrexone-Insensitive
Paradigm� in Behav Neurosci (vol. 104:1, 1990)
pp. 235-238.
24
G.F. Solomon, �Psychoneuroimmunology and Human Immunodeficiency Virus
Infection� in Psychiatr Med (vol. 7:2, 1989)
pp. 47-57.
25
S. Cohen, D.A. Tyrrell, and A.P. Smith, �Psychological Stress and
Susceptibility to the Common Cold� in N Engl J Med
(vol. 325: 9) pp. 606-612.
26
G.F. Solomon, �Emotions, Stress, the Central Nervous System, and Immunity�
in Ann NY Acad Sci (vol. 164:2, 1969) pp.
335-343.
27
P.T. Marucha, J.K. Kiecolt-Glaser, and M. Favagehi, �Mucosal Wound Healing
Is Impaired by Examination Stress� in Psychosom Med
(vol. 60:3, 1998) pp. 362-365.
28
M.S. Harbuz, �Chronic Inflammatory Stress� in
Baillieres Best Pract Res Clin Endocrinal Metab (vol. 13:4, 1999) pp.
555-565.
29
G.F. Solomon, G.H. Ironson, and E.G. Balbin, �Psychoneuroimmunology and
HIV/AIDS� in Ann NY Acad Sci (vol. 917, 2000)
pp.500-504.
30
M. Irwin, �Immune Correlates of Depression� in Adv Exp
Med Biol (vol. 461:1) pp. 1-24.
31
S. Zisook, S.R. Shuchter, M. Irwin, D.F. Darko, P. Sledge, and K. Resovsky,
�Bereavement, Depression, and Immune Function� in
Psychiatry Res (vol. 52:1) pp. 1-10.
32
M. Irwin, T. Patterson, T.L. Smith, C. Caldwell, S.A. Brown, J.C. Gillin et
al., �Reduction of Immune Function in Life Stress and Depression� in
Biol Psychiatry (vol. 27:1, 1990) pp. 22-30.
33
S.R. Lindheim and M.V. Sauer, �Stress and Infertility: �The Chicken or the
Egg?�� in Fertil Steril (vol. 68:2, 1997) pp.
384-385.
34
M.M. Seibel, �Infertility: The Impact of Stress, the Benefit of Counseling�
in J Assist Reprod Genet (vol. 14:4, 1997) pp.
181-183.
35
L.R. Schover, �Recognizing the Stress of Infertility� in
Cleve Clin J Med (vol. 64:4, 1997) pp. 211-214.
36
H. Chiba, E. Mori, Y. Morioka, M. Kashiwaskura, T. Nadaoka, H. Saito et al.,
�Stress of Female Infertility: Relations to Length of Treatment� in
Gynecol Obstet Invest (vol. 43:3, 1997) pp.
171-177.
37
S.K. Wasser, G. Sewall, and M.R. Soules, �Psychosocial Stress as a Cause of
Infertility� in Fertil Steril (vol. 59:3, 1993)
pp. 685-689.
38
J. Shepherd, �Stress Management and Infertility� in
Aust NZ J Obstet Gynaecol (vol. 32:4, 1992) pp. 353-356.
39
M.W. Nortvedt, T. Riise, K.M. Nyland, and B.R. Hanestad, �Type I Interferons
and the Quality of Life of Multiple Sclerosis Patients. Results from a
Clinical Trial on Interferon Alfa-2a� in Mult Scler
(vol. 5, Oct 1999) pp. 317-322.
40
T. Vial and J. Descotes, �Clinical Toxicity of the Interferons� in
Drug Saf (vol. 10:2, Feb 1994) pp. 115-150.
SimpleToRemember.com - Judaism Online |